Epidemiology of Nephrolithiasis varries according to the geographical area & socioeconomic conditions.
ØIn general UTI is believe to be predisposing factor for the urolithiasis.
ØCalcium oxalate stones are associated with chronic diarrhoeal symptoms.
ØMenopause, postmenopausal hormone use & risk of the incident kidney stones.
Menopause is associated with increased urinary calcium excretion which could increase the risk for the development of calcium containing stones.
ØVit c supplementation may increases the urinary oxalate excretion & thus the risk of calcium oxalate stone formation.
ØThe patient with chronic inflammatory bowel disease had evidence of renal stones.
ØA study suggested that sleeping posture has a role in recurrent kidney stone formation because blood flow may be sluggish to the dependent position, allowing crystals to precipitate. Simple behavioural adjustment, such as frequent changes in the position while sleeping, may reduce the recurrent Nephrolithiasis.
ØA study showed that large consumption of dosages of Vit B6 may decrease the incidence of oxalate stone this may be due to the decrease oxalate production.
Theories of stone formation
ØThere are three basic requirement for stone disease to occur.
they are
o A nidus must form
o The nidus must be retained within the urinary tract
o The nidus must grow to sufficient size.
Four major theories have been proposed to explain stone formation and growth.
They are
1) Supersaturation
2) Crystalization / nucleation
3) Reduction of inhibitors
4) Anatomical abnormalities
1) Supersaturation theory:
This theory is based on the binding of salts, which occurs after a certain concentration is obtained. If the salt concentration is less, the compound remains in solution. However if salt concentration exceeds, the compound precipitates. Temperature and the pH of a solution also affect solubility.
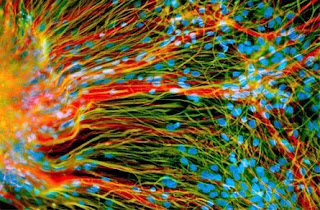
2) Crystallization or Nucleation Theory:
The crystallization or nucleation theory states that when ions or molecules in a dissociated state bind, crystals form. These crystals cluster to form lattice structures. Crystals are nucleated and grow by aggregation.
3) The Inhibitors deficiency theory
Inhibitors are substances that modify or alter crystal growth, thus preventing stone formation. Although urine may be supersaturated with a salt, these inhibitors can prevent stone formation. These molecules work by forming complexes with active surface compounds, which reduces their binding of calcium to oxdiate. Citrate is the most important urinary stone inhibitor, Magnesium, pyrophosphate, nephrocalcin, glycosamine, RNA fragements are other important stone inhibitors. The absence or reduction of these inhibitors can aid in the production of stone formation.
4) Anatomical abnormalities
An anatomic or functional abnormality can cause an obstruction on the flow of urine and the retention of urinary crystals. These crystals anchor to epithelium and cause further crystals to aggregate into stones.
The clinically evident stone has gone through several processes, beginning as an ion in solution. These ions initially become supersaturated in solution. Once their concentration exceeds their solubility, they form crystals and become a nidus for nucleation, aggregation and further growth. If inhibitors are present, stone formation may be prevented, conversely, if there is an absence or reduction in key inhibitors in the urine, then further growth may occur.
Pathogenesis Of Stones
Urinary stones or kidney stone formed when the normal balance of water, salt, minerals and other things found in the urine changes. On the one hand kidney must play an important role in water conservation, but at the same time, minerals with low solubility need to be excreted.
Supersaturation, Nucleation, Aggregation
In general renal stone are of different types, and each type of stone has it’s own group of causes, however, all four types of renal stones share a common pathogenesis that is based essentially upon excessive super saturation of the urine with poorly soluble material.
Under supersaturated condition both homogenous and heterogenous nucleation occurs.
As a result crystal growth proceeds small crystals evolve into large crystals. Alternately many small crystals aggregate to form crystal aggregates.
Urine saturation can be increased by a deficiency of inhibitors of crystal growth, eg. citrate, Magnesium, Pyrophosphate, glycosaminoglycans by dehydration or over excretion of calcium.
Stone formation and Inhibitors
The kidney filter waste products from the blood and add them to the urine that the kidneys produce. When waste materials in the urine do not dissolve completely, crystals & kidney stone are likely to form.
Kidney stone form when there is a high level of calcium (hypercalciuria), oxalate (hyperoxaluria) and uric acid (hyperuricosuria) in the urine; a lack of citrate in the urine or insufficient water in the kidneys to dissolve waste products. The kidneys must maintain an adequate amount of water in the body to remove waste products. If dehydration occurs, high level of substances that do not dissolve completely (eg. Calcium, oxalate, uric acid) may form crystal that slowly build up into kidney stones. Urine normally contain chemicals,
ØCitrate
ØMagnesium
ØPyrophosphate
ØGlycosaminoglycans
These prevent the formation of crystals & low level of these inhibitors can contributes to the formation of kidney stones. Often these citrate is thought to be most important because citrate, or citric acid, is an ordinary component of our diet, present in high amounts in citrus fruits. Citrate binds with calcium in the urine, thereby reducing the amount of calcium available to form calcium oxalate stone.
It also prevent tiny calcium oxalate crystals from growing and massing together into larger stones. Finally, it makes the urine less acidic, which inhibits the developments of both calcium oxalate and uric acid stone.
Magnesium
Magnesium is also one of the crystal inhibitor which present in urine. It act by increasing calcium solubility (especially in the urine) and reducing calcium absorption, magnesium can help to prevent kidney stone specially those composed of calcium oxalate. It is thought that calcium oxalate stone are most likely to form in people who are magnesium deficient, so it may just correcting that deficiency.
Pyrophosphate
Inorganic pyrophosphate is a potent inhibitor which appears to affect calcium phosphate more than calcium oxalate crystals. Other urine inhibitors in urine that appear is glycoproteins, which strongly inhibit the growth of calcium oxalate crystals. As a consequence of the presence of these inhibitors, crystal growth in urine is very slow.
Low level of these inhibitor can contribute to the formation of kidney stone.
Type of kidney stone
·Calcium stones
·Uric acid stones
·Struvite stones
·Cystine stones
·Xanthine stones
Calcium stones
Approximately 85% of stones are composed predominantly of calcium compounds. Common cause of calcium stone production is excess calcium in urine (hypercalciuria), in this excess calcium builds up in the kidney and urine, where it combines with other waste product to form stones.
Calcium stone are composed of calcium that is chemically bound to oxalate (Calcium oxalate) or phosphate (calcium phosphate) of these, calcium oxalate is more common, calcium phosphate stones typically occur in patients with metabolic or hormonal disorders such as hyperparathyroidism and renal tubular acidosis.
Uric acid stones
About 7-10% of stone are made up of uric acid, which is actually crystal that is endproduct of purine metabolism, a nitrogen compound found in the proteins. These stone form because the urine becomes supersaturated with uric acid. Frequently urinary pH is very low and at these low pH value (5.4 or below) undissociated uric acid is very insoluble leads to formation of uric acid stone.
Struvite stone
Struvite stone made up of magnesium ammonium phosphate, occur more commonly in women, usually in presence of a urinary tract infection with urease-producing bacteria. The bacteria (often staphylococcus, Klebsiella, pseudomonas, proteus species) utilize urea in the urine to form ammonia and carbondioxide the ammonia is changed to ammonium which in turn, raises the urine pH and becomes available for the formation of magnesium ammonium phosphate crystals (struvite)
As the urine pH increases, phosphate becomes less soluble
Cystine stone
Cystine is an amino acid in protein that does not dissolve well. Some people with inherited conditions that result in large amount of cystine in urine. This condition called cystinuria causes cystine stone that are difficult to treat & requires life-long therapy.
Cystine stone, account for about 1 to 3% of all renal calculi. Cystine stones develop from genetic defects that cause abnormal transport of amino acids in the kidney and gastrointestinal system leading to a build-up of cystine, one of the amino acids.
Xanthine stones
An increased urinary excretion of xanthine may cause the formation of xanthine stones. In some cases, xanthine stones may develop in patient being treated with allopurinol for gout.
Stone composition
Components
Percentage
Calcium stone (Oxalate & phosphate)
77%
Uric acid stone
7 – 10%
Struvite stone
8%
Cystine stone
1 - 3%
Others
4%
Etiology Of Renal Calculus
Kidney stone form when there is a decrease in urine volume or an excess of stone forming substances in the urine.
·Dehydration through reduce fluid intake or strenuous exercise without adequate fluid replacement increases the risk of kidney stones.
·Obstruction to the flow of urine can also lead to stone formation.
A number of different conditions on lead to kidney stones
1) Gout : Result in an increased amount of uric acid in the urine and can lead to the formation of uric acid stones.
2) Hypercalciuria : (high calcium in urine)
Another inherited condition, causes stone in more than half of cases.
In this condition too much calcium is absorbed from food and excreted into the urine, where it may form calcium oxalate or calcium phosphate stones.
3) Other conditions associated with an increased risk of kidney stone include
·Hyperparathyroidism is one of the metabolic disorders results in a great increase in the elimination of calcium in the urine.
·Renal tubular acidosis, Kidney diseases, is an inherited condition in which the kidneys are unable to excrete acids.
·Certain inherited metabolic conditions including cystinuria & hyperoxaluria.
4) People with inflammatory bowel disease or who have had an intestinal bypass or ostomy surgery are also more likely to develop kidney stone.
5) Some medications also raise the risk of kidney stones. These medication include some diuretics, calcium containing antacids, and the protease inhibitor crixivan (indinavir), a drug used to treat HIV infection.
Risk Factors For Nephrolithiasis
Several factors increases the risk for developing kidney stones, including
·Inadequate fluid intake and dehydration.
·Reduce urinary flow and volume.
·Use of certain medication (eg Vitamin C, calcium)
·Diet high in oxalate or sodium.
Chemical risk factors include high levels of the following in the urine
·Calcium (hypercalciuria)
·Cystine (cystinuria; caused by a genetic disorder)
·Oxalate (hyperoxaluria)
·Uric acid (hyperuricosuria)
·Sodium (hypernatremia)
A low level of citrate is a risk factor for hypocitraturia.
The following medical conditions are also risk factos. Gout, hyperparathyroidism, hypertension, chronic diarrhoea, renal tubular acidosis, recurrent UTI infection.
Nephrolithiasis symptoms & signs
ò Flank pain or back pain
·On one or both side
·Progressive
·Severe
·Colicky (Spasm – like)
·May radiate or move to lower in flank, pelvis, groing, genitals.
ò Nausea, vomiting
ò Urinary frequency / urgency, increased (persistent urge to urinate)
ò Blood in the urine
ò Abdominal pain
ò Painful urination
ò Excessive urination at night
ò Urinary hesitancy
ò Testicle pain
ò Groin pain
ò Fever
ò Chills
ò Abnormal urine color
Nephrolithiasis prevention
If there is a history of stones, fluids should be encouraged to produce adequate amounts of dilute urine (usually 6 to 8 glasses of water per day). Depending on the type of stone, medications or other measures may be recommended to prevent recurrence.
Diagnosis
Kidney stones are easy to diagnose for those with a sudden onset of pain, blood in the urine and stones that show on x-ray. For others diagnosis is less straight forward as:-
· Plain x-rays do not ‘see’ stones not made of calcium, like those containing uric acid. Small stones and those in front of bones do not show up either.
· Intravenous urography (IVU) is an older test that may be used for stones that x-ray cannot show. Dye is injected into a vein and x-ray studies are taken as it passes through the kidneys. Any problems with the passage of urine out of the body also show.
· CT scanning shows all stones well
· Ultrasound scanning is less good at seeing stones but can show if a blockage is present. It is an option in pregnancy.
· Levels of calcium and uric acid in the blood will be examined
· Any stone passed out of or removed from the body is analysed to identify the constitutents.
Where people repeatedly form stones there will be
· A full metabolic evaluation and measurement of certain substances in the urine and blood
· A dietary assessment.
Treatment
Treatments aim is to relieve symptoms, deal with complications and prevent the formation of more stones. Treatment varies depending on the type of stone and the extent of symptoms and or complications. Hospitalization may be required if symptoms are severe.
·Drink enough fluid to produce a high urinary output. Water is encouraged, at least 6 to 8 glasses per day.
·Management of pain: Analgesics may be needed to control renal colic. Sever pain may require narcotic analgesics.
·Medication to relieve any nausea.
·Intravenous fluids may be given if needed.
·Depending on the type of stone, Medications may be given to decrease stone formation and or aid in the breakdown and excretion of the material causing the stone. These may include such medications as diuretics, phosphate solutions, allopurinol (for uric acid stones) antibiotics (for struvite stone) and medication that alkalinize the urine such as sodium bicarbonate or sodium citrate.
·The diagnosis will be confirmed using the tests
oIntravenous urography (IVU)
oIntravenous pyelogram (IVP)
oCT scanning
oUltrasound scanning
oSmall stones (Smaller than 5mm) usually pass by themselves within 72 hours. Any stones should be kept for analysis.
o Tests are repeated to confirm that the stone has passed out of the body.
Stones of upto 9mm in size may pass, but those larger will not and more active treatment is needed. Sometime surgical removal may be required.
o Lithotripsy may be an alternative to surgery.
o Extracorporeal shockwave lithotripsy (ESWL) is a procedure used to shatter simple stones in the kidney or upper urinary tract.
Ultrasonic waves are passed through the body until they strike the dense stones. Pulses of sonic wave pulverize the stones, which are then more easily passed through the ureter and out of the body in the urine.
o If necessary, stone can be removed using the techniques of ‘keyhole’ surgery. This procedure is known as ‘nephrolithotomy’.
o Staghorn calculi or other very large stones may require conventional surgery